Are you looking for a
Medical Solutions?
Schedule your company strategy right session now
About Us
We are a medical billing company that provides 24-hour medical billing services and provides end-to-end medical billing solutions to physicians, hospitals, medical institutions, and group practices. Backed by the latest technologies and purpose-driven approach, we leverage customized Revenue Cycle Management (RCM) solutions that allow hospitals and clinics to attract revenue and reduce administrative burden or losses.
Who Are We

Medical Coding & Billing
Our billing and coding professionals have extensive knowledge of Medicare, HIPAA, and Medicaid rules, as well as hands-on experience with them.
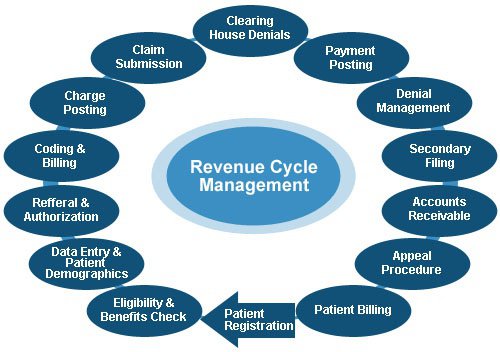
Revenue Cycle Management
Our Revenue Cycle Solutions provides hospitals, emergency rooms, urgent care centres, and physicians of all specialties with comprehensive medical billing and coding services.
Our industry-leading technology platform, Elevate^, gives you real-time data visibility and actionable insights to support your risk and quality initiatives.
W3medcare is a one-stop-shop for all primary health care services, including eligibility checks, coding, billing, AR follow-up, collections, denial management, collections, to name a few. We provide cost-effective and dependable services that are in line with current healthcare trends.
Our Services
FOCUSED ON CREATING A MORE EFFICIENT HEALTHCARE SYSTEM
Our workflow and reporting systems are built to empower suppliers and physicians by providing them control over their billing and allowing them to see how much money their practice makes. We develop a relationship with the complete in-house team, not just the supplier so that the practice functions as a whole rather than as individual parts.
What Our Client Say
Many of our clients have built wonderful partnerships with us, and we are grateful for that. And we’ve developed an actual connection with them in addition to professional relationships. Here’s what they’re saying about us.
W3medcare has worked with a variety of providers, ranging from small to major clinics, over the course of a decade in the medical billing sector. We’ve successfully handled a wide range of billing requirements for providers. They’re fantastic. Their professionals supplied expert advice and assistance in a personal and timely manner.
W3medcare is a company I would suggest to clinics and hospitals looking to outsource medical billing.
I’d want to offer my heartfelt gratitude to W3medcare for the commitment you’ve shown to our firm; you’ve been a true blessing, and I appreciate you. You’re doing an excellent job, which gives us more time to focus on the client in areas where we could only glance. The executives are so professional yet cheerful that my front desk staff calls them with every billing question, and they always respond with the same enthusiasm. I was able to cut costs by 30%.
Thank you again for your kind assistance!
W3medcare is to thank for this one. I was initially depressed and seeking a trustworthy partner to assist me with my medical revenue. In just 5 months, my revenue rose by 30%, my patients appreciate their claims being paid correctly, and I was able to add two more physicians to my practise.
Our Blog
Find out about the latest trends, insights, and digital obsessions in the medical industry from the leading healthcare experts
Over 150 Healthcare Organizations Partner with W3medcare
Our long-standing evangelists can tell you more